Laser Cholesteatoma Surgery
Why cholesteatoma is removed more effectively when a laser is used and how lasers help preserve hearing in cholesteatoma more effectively than any other technique.
In most cases, cholesteatoma results from abnormal growth of the skin of the ear drum into the skull.
The resulting sac continually generates skin cells. These stagnate causing relentless or recurrent ear discharge. The inflammation caused by the infected skin causes erosion of the structures within the skull.
Cholesteatoma is the accumulation of skin debris within the middle ear.
The middle ear occupies much of the temporal bone which is the main bone on each side of the base of the skull.
Cholesteatoma does not occur anywhere else.
In addition to ear discharge a patient with cholesteatoma may notice symptoms caused by destruction of the structures within the skull. The commonest of these symptoms is hearing loss.
Less common symptoms include dizzyness, tinnitus and facial weakness. Most people are surprised to learn that cholesteatoma rarely causes pain.
If an abscess forms, it causes pain and swelling around the ear and can result in meningitis or other infection of the brain. When cholesteatoma is neglected such serious complications can cause death.
Cholesteatoma causes inflammation. Inflammation causes erosion of bone, so the cholesteatoma progressively enlarges.
It also causes scarring so that the cholesteatoma becomes firmly attached to the structures in the temporal bone.
At any time, the indolent suppuration of the dead skin within the cholesteatoma may erupt into an abscess.

Other ear disorders, such as ear drum perforation and ear canal infection also cause hearing loss and ear discharge.
The following features should raise suspicion that cholesteatoma is present:
- Relentless ear discharge despite treatment
- Recurrent ear discharge despite treatment
- Foul smelling ear discharge
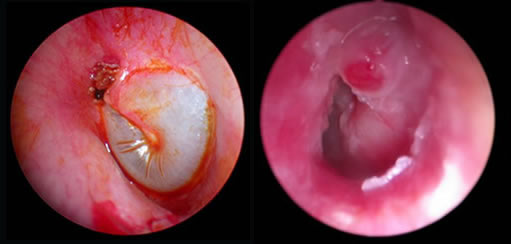
Cholesteatoma is usually diagnosed on careful inspection of the eardrum. This may be obvious or it may be subtle. It often requires the ear to be competely clean, which may require specialist skills and equipment.
On rare occasions, scans are required to diagnose or confirm the presence of cholesteatoma

Most of the temporal bone is occupied by the air spaces of the middle ear. This air space is neede to allow the ear drum to vibrate and transmit sound.
The ear canal, ear drum and hearing bones are also housed within the temporal bone. Their role is also to transmit sound through to the inner ear.
The inner ear, which has two parts, the cochlea (for hearing) and the vestibule (for balance) lies deep within the temporal bone.
Nerves from the brain to the face and neck run through the temporal bone.
Major bood vessels to and from the brain also run through the temporal bone.
Cholesteatoma is an abnormal physical structure. It cannot be removed with medicines.
As it is progressive, it requires removal, which means surgery.
All cholesteatoma should be surgically removed if the patient is fit enough for anaesthetic.
Cholesteatoma surgery has two conflicting aims. Getting the balance between these is very difficult. This is the reason why you should consider carefully who performs your cholesteatoma surgery.
The conflicting aims of cholesteatoma surgery are:
- To completely remove (and prevent the recurrence) of cholesteatoma.
- To maintain or restore the normal function of the structures of the temporal bone.
The conflict arises because:
- The former is facilitated by wide removal of all the structures of the temporal bone.
- The latter is facilitated by preservation of the structures of the temporal bone.
There are many techniques currently used to try to achieve these aims. Older techniques tend to be heavily biased towards achieving the first aim at the cost of the second.
This is the reason why you should consider carefully who performs your cholesteatoma surgery.
Mr Hamilton has proposed that four outcomes should be recorded to measure the effectiveness of cholesteatoma surgery.
- Complete removal of cholesteatoma
- No new growth of cholesteatoma
- Dry ear, even when washing or swimming
- Socially useful hearing
The first two assess whether the disease has been completely removed. The latter pair assess whether the ear is functioning normally. Each is a simple yes/no answer.
Take a look at how well cholesteatoma is completely removed in one operation:
Famous and dedicated surgeons who have audited and published their work often have residual cholesteatoma rates of 15-30 per cent.
Is this necessarily a measure of individual failure? If even the most skilled surgeons leave this amount of disease, the problem resides more with the limitations imposed by the surgical instruments than with the dexterity of the surgeons:
Conventional instruments are not up to the task of completely clearing all cholesteatoma.
Lasers vaporise disease and therefore are:
- simple to use
- cause no movement
- stop bleeding
Some lasers can be transmitted along fibres. These can guide the laser energy around corners. In cholesteatoma surgery, this means that the laser can be guided around the many obstacles in the temporal bone.
Some surgeons feel that endoscopes may help by improving inspection and image capture of cholesteatoma in regions of complex anatomy. However, the benefit of endoscopy in cholesteatoma surgery is limited as:
- endoscopes are not actually used for removing disease;
- the surgeon holding an endoscope has only one free hand to perform surgery;
- endoscopes are difficult to use with bleeding tissues.
| problems encountered during cholesteatoma surgery | conventional steel instruments | fibre-guided laser |
|---|---|---|
| cochlea damaged by movement of hearing bones | movement needed to remove disease | no movement involved in disease |
| many obstacles | can work around corners with angled instruments | can be guided around corners by optical fibre or off mirror |
| inflamed tissues full of blood vessels |
dissection worsens bleeding | laser stops bleeding |
| complex anatomy | requires dexterity especially around corners | point and shoot |
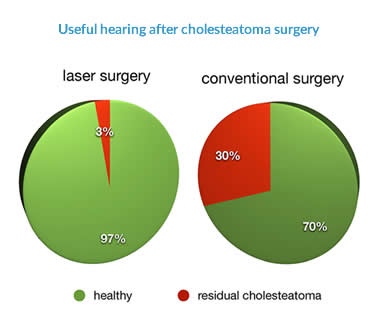
Mr Hamilton compared the complete clearance of cholesteatoma in two hospitals, one with a laser and one without. He did this by checking whether there was any residual cholesteatoma at a second operation.
The flow chart shows how patients were involved in the study:
When Mr Hamilton relied on conventional instruments, he failed to clear the disease completely at the same rate as other good surgeons. When he used the laser as well, the rate at which he failed to clear the disease completely was reduced by a whole order of magnitude.
The laser does not require movement to remove cholesteatoma. This means that an entirely new approach can be adopted to the treatment of firmly adherent cholesteatoma on the hearing bones.
Previously it was necessary to remove the hearing bones with the cholesteatoma, in order to protect the delicate inner ear from damage.
Now the laser can remove firmly adherent cholesteatoma from the hearing bones without movement and thereby without placing the inner ear at risk
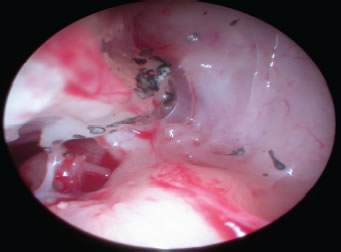
Cholesteatoma can be lasered from the ossicles themselves without movement.
The ossicles also present a barrier to removal of cholesteatoma.
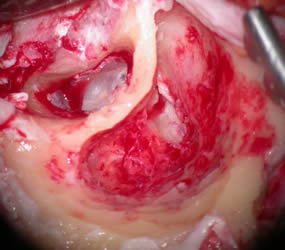
A special view, the "orthogonal" view, has been developed to get to the cholesteatoma on the other side of the ossicles: this enables a direct view of the deep side of the ossicles, the facial nerve and the gap in between which Mr Hamilton has termed the epitympanic gutter. This view protects the facial nerve and the hearing bones as the cholesteatoma is removed.

- The area is approached using the orthogonal view.
- The facial nerve is identified and protected.
- The laser used on the ossicular side only, to protect the cochlea.
- Steel instruments only are used on the facial nerve side, to protect the nerve.
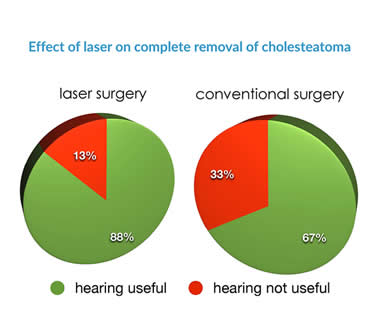
Mr Hamilton compared the hearing of two groups of patients after cholesteatoma surgery. One group had conventional treatment of the hearing bones, with reconstruction after removal of bones to facilitate surgery. The other group had new, laser-assisted "functional" surgery, in which cholesteatoma was removed from and around the hearing bones, which were left in place.
Analysis of the results showed that the risk of poor hearing in the conventional group was approximately 3 times higher than the risk of poor hearing in the laser group.
Lasers are better suited to the removal of cholesteatoma than conventional instruments.
Over the last decade Mr Hamilton has provided evidence that:
- Cholesteatoma is removed more effectively when a laser is used
- Lasers provide an opportunity to preserve hearing more effectively than any other technique
To achieve these outcomes has required the development of a new approach to cholesteatoma surgery.
This has required new technical terms and ultimately a new operation, Functional Orthogonal Cholesteatoma Surgery.